Are there differences in Toxicity between oral ingestion of marijuana and Smoking?
Presented at the Neu Psyco 2014 conference, Nov. 18th, Havana, Cuba
During the past year, the legalization of marijuana (MJ) for medical purposes in the US has greatly increased the use of MJ among adults and teens. Medical marijuana “dispensaries” have opened their doors to patients with legitimate prescriptions for cannabis-containing products, including those that can be smoked, vaporized, placed under the tongue, and eaten in cookies, candy and snack-like items. Unfortunately, most of the earlier research on MJ focused on administering MJ by smoking, and little recent research was conducted on the administration of MJ by the oral route. This knowledge deficit has now come back to haunt us, as the media have reported many serious adverse reactions to MJ, in people who have consumed it by the oral route.
In May of 2014, USA Today published a report of two men who had eaten marijuana in a cookie or candy and had psychotic reactions. One 19 year-old college student ate a marijuana-laced cookie and shortly thereafter began rambling incoherently and subsequently jumped to his death from the balcony of a Denver, CO hotel. The Denver coroner listed marijuana intoxication as a significant factor in his death, and reported that he had a blood level of 7.2 ng/ml, (equivalent to 14 ng/ml plasma concentration) a concentration that would be found approximately 2 hours after smoking a 3.55% THC marijuana cigarette.
A second man developed hallucinations and rambling speech after eating marijuana-containing candy and concomitant ingestion of an unidentified prescription medication, and in the midst of an apparent psychotic break, fatally shot his wife while she was calling 911 for help. What was the common denominator in these two cases? Both men consumed the MJ orally, rather than smoking it.
In early September, five high school students in the San Francisco, CA area, ages 14-16, became ill after eating brownies that had been laced with MJ. Three developed nausea and vomiting and two became unconscious and were hospitalized. The brownies were sold to the students by a classmate. There are no toxicology results indicating if the brownies contained other “drugs” or if they contained only MJ.
While nausea, vomiting, lightheadedness and occasional adverse psychiatric or paranoid reactions have been associated with smoking MJ since the 1960s, reports of severe alterations in consciousness requiring hospitalization have been quite rare. If the brownies contained only MJ (THC), aside from overdosage, why did two of the students lose consciousness and require hospitalization? The answer may reside in the differences in effect between orally-ingested MJ and smoked.
Smoked marijuana is absorbed into the pulmonary circulation, and returned to the heart through the pulmonary vein. From the heart, it is distributed systemically, without passing through the liver. However, orally ingested THC is subject both to transmural absorption and metabolism in the G.I. tract and “first-pass” hepatic metabolism as it passes through the liver. As a result, THC is metabolized more extensively by the oral route, leading to the synthesis of a much larger amount of 11-OH-THC than is generally formed following smoking. The 11-OH-THC metabolite is psychopharmacologically active and can combine its psychotropic effects with those of THC to produce a more robust psychotropic effect in the CNS. The magnitude of the effect of the combined 11-OH-THC and THC most likely was the cause of the psychotic reactions and loss of consciousness described in the cases reported above.
In 1973, Lemberger demonstrated the psychotropic effects of the 11-OH-THC metabolite when he administered tritiated IV doses of THC, 11-OH-THC (formulated in ethanol) or ethanol, under blinded conditions, to nine casual marijuana users. Following the administration of 1 mg of 11-OH-THC, a marked tachycardia and euphoric “high” occurred in 3-5 minutes, and psychologic effects correlated well with 11-OH-THC plasma levels. However, IV administration of 1 mg of THC required a latency period of 10-20 minutes after IV administration, before the peak subjective “high” was reported by the subjects. The authors concluded these results indicated that the psychologic effects of THC were, at least partially mediated through the 11-OH-THC metabolite, and that the latency period was indicative of the time required to convert the THC to 11-OH-THC.
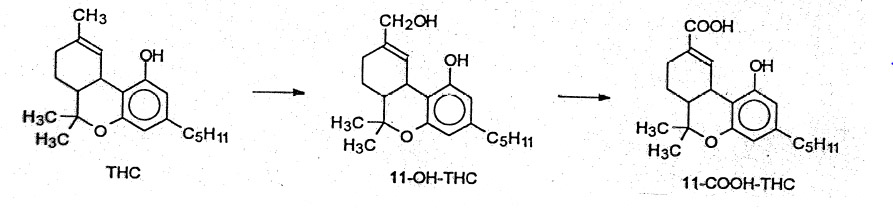
Tetrahydrocannabinol (THC), shown in Figure 1, normally undergoes oxidation to the 11-OH-THC metabolite by the polymorphic CYP2C9 enzyme, which is finally oxidized to the inactive, 11-nor – 9-carboxy-THC (THC-COOH) acid which appears in the blood and urine. When THC is smoked, far less 11-OH-THC is formed and the magnitude of the effect is less than with 11-OH-THC and THC together.
A review of the package insert for the FDA-approved synthetic Δ9– tetrahydrocannabinol, dronabinol, indicated that during clinical trials, adverse psychotropic effects similar to those reported above, occurred in 3-10% of patients and that the dronabinol was the most probable cause of the dizziness, euphoria, paranoid reaction, somnolence and abnormal thinking reported in the manufacturer’s labeling. After marketing, severe overdosage of dronabinol was reported to cause panic reactions in apprehensive patients and other significant CNS symptoms which were not specifically defined.
Key Words: acute psychotic reactions; hepatic metabolism; route of administration.
References
- Marijuana treats pose hidden dangers. Trevor Hughes. USA Today Weekend, 1A-2A, May 9-11, 2014.
- emberger, L, Martz, R., Roda, R. et al. Comparative Pharmacology of Δ9– tetrahydrocannabinol and its metabolite, 11-OH- Δ9– tetrahydrocannabinol. J. Clin. Investigation, 1973;2411-2417.
- Sachse-Seeboth, C., Pfell, J., Meineke, I., et al. Interindividual Variation in the Pharmacokinetics of Δ9-Tetrahydrocannabinol as related to Genetic Polymorphism in CYP2C9. Clin. Pharmacol. Therap. 2009; 85(3):273-276.
- Huestis, Marilyn A., Henningfield, Jack E. and Cone, Edward J.: Blood Cannabinoids. I. Absorption of THC and formation of 11-OH-THC and THCCOOH During and After Smoking Marijuana. J. Analyt. Tox. 1992; 16:276-282.
- Marinol ® (dronabinol) Capsules, manufacturer’s package insert, Banner Pharmacaps, Inc., High Point, NC, for AbbVie Inc., N. Chicago, IL, February, 2013
- Papanti, D., Schifano, F., Botteon G. et al., “Spiceophrenia”: a systematic overview of “Spice”-related psychopathological issues and a case report. Hum. Psychopharmacol Clin Exp 2013; 28: 379–389. Published online in Wiley Online Library (Wileyonlinelibrary.com) DOI: 10.1002/hup.2312).